All kinds of Wound Management
Wound management involves a comprehensive approach to caring for wounds of various types, sizes, and etiologies to promote optimal healing and prevent complications. Different wounds require different management strategies, which may include:
-
Acute Wounds:
- Clean Wounds: Clean wounds with minimal contamination are typically managed with simple wound care techniques, such as cleaning with saline solution, applying a sterile dressing, and monitoring for signs of infection.
- Contaminated Wounds: Wounds with foreign material or contamination may require thorough irrigation with saline or antiseptic solutions to remove debris and reduce the risk of infection.
- Lacerations and Incisions: Lacerations and surgical incisions may require wound closure using sutures, staples, or adhesive strips to approximate the wound edges and promote healing.
- Bite Wounds: Animal bites or human bites often require thorough cleaning, debridement of devitalized tissue, and prophylactic antibiotics to prevent infection.
-
Chronic Wounds:
- Pressure Ulcers: Pressure ulcers, also known as bedsores, require relieving pressure on the affected area, frequent repositioning, and specialized wound dressings to promote healing and prevent further tissue damage.
- Diabetic Foot Ulcers: Diabetic foot ulcers require meticulous wound care, offloading pressure from the affected area, management of blood glucose levels, and possibly surgical debridement or advanced wound therapies.
- Venous Ulcers: Venous ulcers associated with chronic venous insufficiency may require compression therapy, wound debridement, and topical wound care to facilitate healing and prevent recurrence.
- Arterial Ulcers: Arterial ulcers associated with peripheral arterial disease require optimizing blood flow to the affected area, often through revascularization procedures, along with wound care to promote healing.
-
Burn Wounds:
- Superficial Burns: Superficial burns, such as first-degree burns, typically heal with conservative wound care, including cooling the affected area, applying topical ointments, and protecting the wound from further trauma.
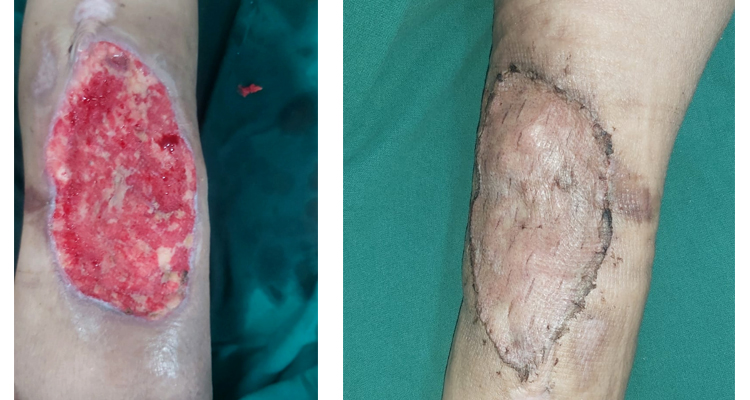
- Partial-Thickness Burns: Partial-thickness burns, such as second-degree burns, may require debridement of blistered or necrotic tissue, application of topical antimicrobial agents, and specialized dressings to facilitate wound healing.
- Full-Thickness Burns: Full-thickness burns, including third-degree burns, often require surgical intervention, such as skin grafting or tissue flap reconstruction, along with intensive wound care and rehabilitation.
-
Surgical Wounds:
- Postoperative Wounds: Surgical wounds require careful monitoring for signs of infection, proper wound care techniques, and adherence to surgical incision care protocols to minimize the risk of complications, such as dehiscence or surgical site infections.
- Wound Dressings: Various types of wound dressings may be used depending on the type and stage of the wound, including gauze dressings, foam dressings, hydrocolloid dressings, alginate dressings, and transparent films.
-
Advanced Wound Therapies:
- Negative Pressure Wound Therapy (NPWT): NPWT involves applying negative pressure to the wound bed to promote wound healing, reduce edema, and enhance granulation tissue formation.
- Bioengineered Skin Substitutes: Bioengineered skin substitutes, such as dermal matrices or skin graft substitutes, may be used to promote wound closure and tissue regeneration in complex or chronic wounds.
- Hyperbaric Oxygen Therapy (HBOT): HBOT involves exposing the patient to 100% oxygen at increased atmospheric pressure, which can promote wound healing by increasing oxygen delivery to hypoxic tissues and enhancing angiogenesis.
-
Infection Management:
- Antibiotic Therapy: Systemic or topical antibiotics may be prescribed to treat or prevent wound infections, particularly in contaminated or high-risk wounds.
- Wound Cultures: Wound cultures may be obtained to identify the causative organisms and guide antibiotic selection in infected wounds.
- Debridement: Debridement of necrotic or infected tissue is essential for controlling infection and promoting wound healing. Debridement methods include sharp debridement, enzymatic debridement, mechanical debridement, and autolytic debridement.
-
Nutritional Support: Adequate nutrition is essential for wound healing. Patients with chronic or complex wounds may require nutritional supplementation, dietary counseling, and assessment of micronutrient deficiencies to optimize wound healing.
-
Pain Management: Pain associated with wound care procedures and wound-related discomfort should be addressed through appropriate analgesic measures, such as oral medications, topical anesthetics, or non-pharmacologic interventions.
Effective wound management requires a multidisciplinary approach involving healthcare professionals with expertise in wound care, including physicians, nurses, wound care specialists, physical therapists, and dietitians. The choice of wound management strategies depends on various factors, including the type, location, size, and severity of the wound, as well as the patient's overall health status and preferences. Regular assessment and ongoing monitoring of wounds are essential for identifying any changes or complications and adjusting the treatment plan accordingly.
Book Appointment